Sleep apnea monitoring plays a key role for those with bad sleep and health risks. If you are looking to check your sleep with no need for a sleep lab, this guide is what you need. Here, we show the steps to set up sleep apnea monitoring right at home, helping to gather the details for a good diagnosis.
We cover what sleep apnea is and why it’s important. You will find details on different types of home sleep monitoring tools. You learn how to set your monitoring gear properly, use best methods for accurate results, and go over findings with your doctor. By the finish, you will be ready to take charge of your sleep health and start your path to better sleep and wellness.
Understanding Sleep Apnea and Its Importance
Sleep apnea is a significant sleep disorder. It features repeated pauses in breathing while asleep. Obstructive sleep apnea (OSA) is the most common form. This occurs when throat muscles relax too much, causing airway blockage. It disrupts sleep, hindering deep restorative cycles.
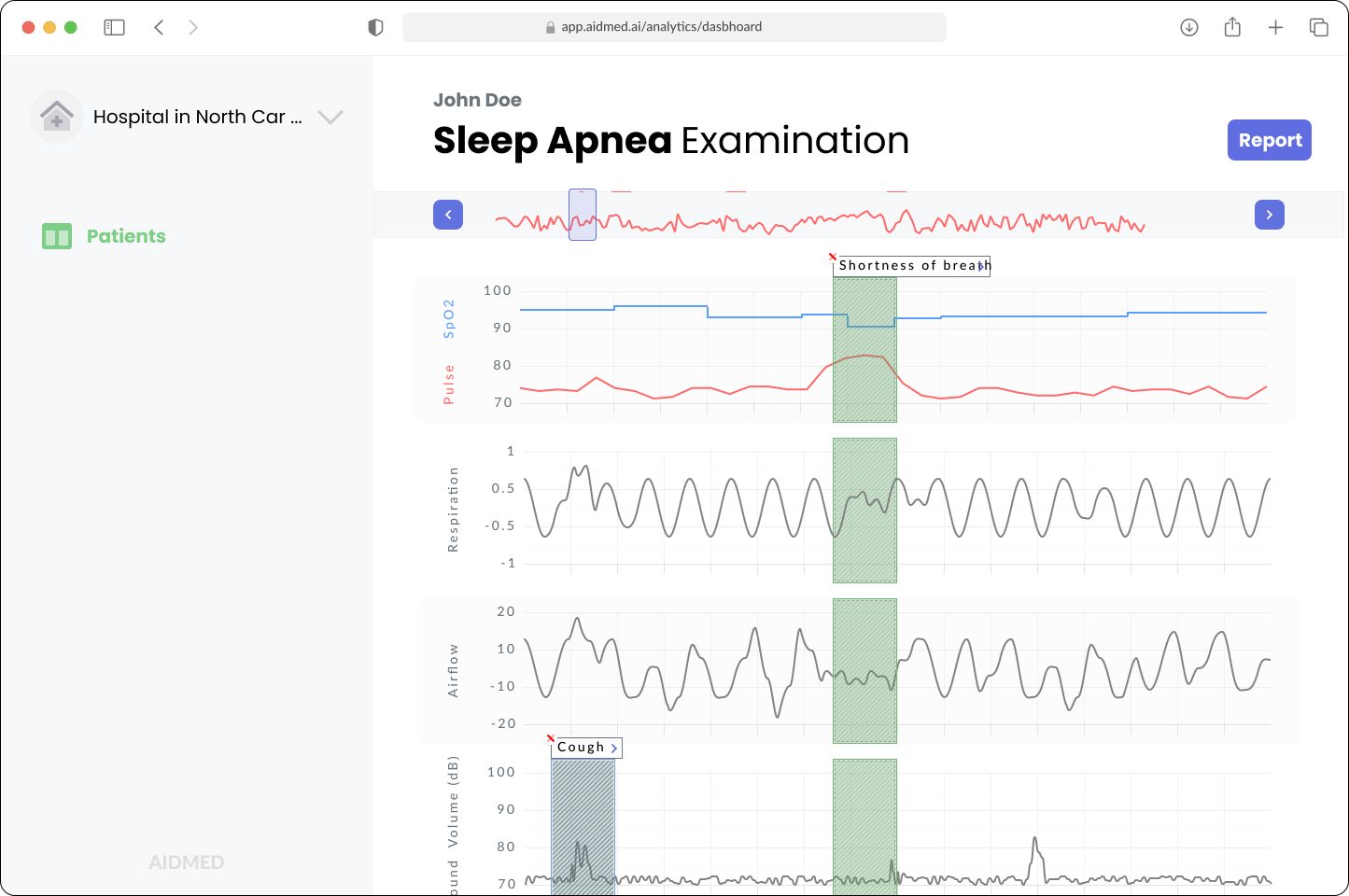
Example of obstructive sleep apnea examination
People may stop breathing briefly when sleep apnea occurs. These pauses can last from seconds to over a minute. Such interruptions lower blood oxygen levels. This added strain affects the cardiovascular system. Untreated sleep apnea causes serious health problems. This includes hypertension, heart disease, and arrhythmias.
A major concern with sleep apnea is its daytime effects. Many report excessive fatigue each day. It reduces productivity and increases accident risks at work and driving. Also, long-term sleep disruption degrades life quality. It impacts mood, cognition, and emotional health substantially.
About 20% of adults may have sleep apnea. Many stay undiagnosed. This highlights the value of sleep apnea monitoring. Monitoring sleep patterns and oxygen levels identifies those needing treatment. They gain useful health insights and can pursue treatments.
With knowledge of sleep apnea's health effects, exploring home sleep apnea testing setups is the next move.
Home Sleep Apnea Monitoring Overview
Home Sleep Apnea Monitoring has gained traction for diagnosing sleep apnea at home. Unlike traditional tests in sleep centers, this method lets patients monitor their sleep without overnight stays. Patients wear portable monitors that collect data on airflow, breathing, and oxygen levels during sleep.
One major plus of sleep apnea monitoring at home is its convenience. Patients follow their regular bedtime routines, which lower anxiety and gives more accurate results than labs might. Home testing removes scheduling hassles and travel problems that keep people from getting evaluations.
Studies show home sleep apnea monitoring can accurately find Obstructive Sleep Apnea in many cases, especially in those at higher risk. The results are reliable, matching those from in-lab tests, especially with moderate to severe cases. Home testing helps those who may not want standard studies.
HSATs track physiological markers that point to sleep apnea events. They evaluate apnea, hypopnea, and overall sleep quality. Healthcare providers get the data they need to confirm or dismiss a sleep apnea diagnosis. This method makes accessing sleep studies easier and speeds up diagnosis.
Now, let’s look at how to set up your home sleep apnea monitoring device effectively.
Setting Up Your Home Sleep Monitoring Device
Setting up your home sleep apnea monitoring device is key for effective results. This guide helps you configure your device for accurate sleep pattern assessments.
-
Review Your Device Instructions. Start by reading the user manual that comes with your sleep monitoring device, like the ApneaLink. Knowing how it works is vital for a successful setup.
-
Device Assembly. Assemble your device carefully according to provided instructions. This includes attaching sensors and belts to track airflow and other metrics. Make sure every connection is secure to prevent disconnections at night.
-
Wearing the Device. After assembly, wear the device as directed. The ApneaLink normally uses a nasal cannula or sensor under your nose to sense breathing. Adjust straps for comfort, avoiding pressure during sleep.
-
Comfort and Responsiveness. Comfort is crucial for sleep apnea monitoring. Place the device in a way that allows movement at night. Testing it while awake can help ensure the fit is right, snug but not overly tight.
-
Check the Settings. Check that the device is turned on and properly set. Some devices let you calibrate or choose specific monitoring settings. Proper configuration can heavily influence the accuracy of sleep data.
-
Prepare for Sleep. Before bed, ensure your environment is quiet, dark, and cool. Maintain a regular sleep schedule leading to the monitoring night for best results. Use blackout curtains, eye masks, earplugs, or white noise machines to keep distractions away. Avoid caffeine and alcohol for at least 24 hours before testing. Caffeine hinders your sleep, while alcohol can disturb sleep patterns and hide sleep apnea symptoms, causing unreliable results. Go to bed and wake up at the same time daily for a few days before your test. A steady routine prepares your body and lets the device capture precise sleep data, make sure your sleep patterns are normal.
-
Understanding Data Collection. Throughout the night, the device gathers data on breathing and oxygen levels. Follow proper procedures to prevent inaccuracies caused by movement or device removal during sleep. Keeping a log of disturbances may help your healthcare provider with results evaluations.
-
Final Checks. Lastly, check that all leads are correctly placed, and ensure the device is functional. Once set, rest easy knowing you’re ready for a monitored sleep.
Your setup quality impacts collected data and your understanding of sleep apnea management. Transitioning to learn about available home sleep monitors will prepare you for your next steps in sleep apnea treatment.
Types of Home Sleep Monitors Available
When it comes to sleep apnea monitoring, choosing the right device is key to gather good information on your sleep patterns and apnea events. A variety of home sleep monitors exist, each with unique features and different levels of complexity. The main types include Type II, Type III, and Type IV monitors.
Type II monitors
Type II monitors are the most detailed choice, often integrating multiple sensors for data collection on airflow, respiratory effort, and blood oxygen levels. These devices aid in assessing and diagnosing sleep apnea accurately, resulting in a thorough analysis of sleep stages plus disturbances.
Type III monitors
Type III monitors have limited features, using fewer sensors and mainly focusing on airflow and blood oxygen saturation. While they still help, Type III devices may not provide as comprehensive details as Type II monitors. They suit those with moderate to severe sleep apnea who do need rich data collection.
Type IV monitors
Type IV monitors are the simplest. They often consist of devices needing less setup, limited usually to measuring airflow or blood oxygen levels. These are fit for screening only. Users must understand these monitors’ limitations concerning their condition's severity.
When selecting a home sleep monitor, it’s wise to think over the suspected severity of your apnea. In case of severe symptoms, a Type II monitor will deliver the best data for diagnosis. If symptoms mild are, then Type III or IV monitor should be just fine.
Also, evaluating features like data accuracy and ease of use is important. Some devices connect to apps on smartphones to visualize data; others may need more manual data analysis. Picking the right home sleep monitor is vital in tracking sleep apnea and improving sleep health management.
With the right equipment, you'll have an effective setup for monitoring sleep apnea at home. Next, let’s look into best practices for conducting effective at-home sleep tests to ensure accuracy and reliability of results.
Evaluating Sleep Study Results
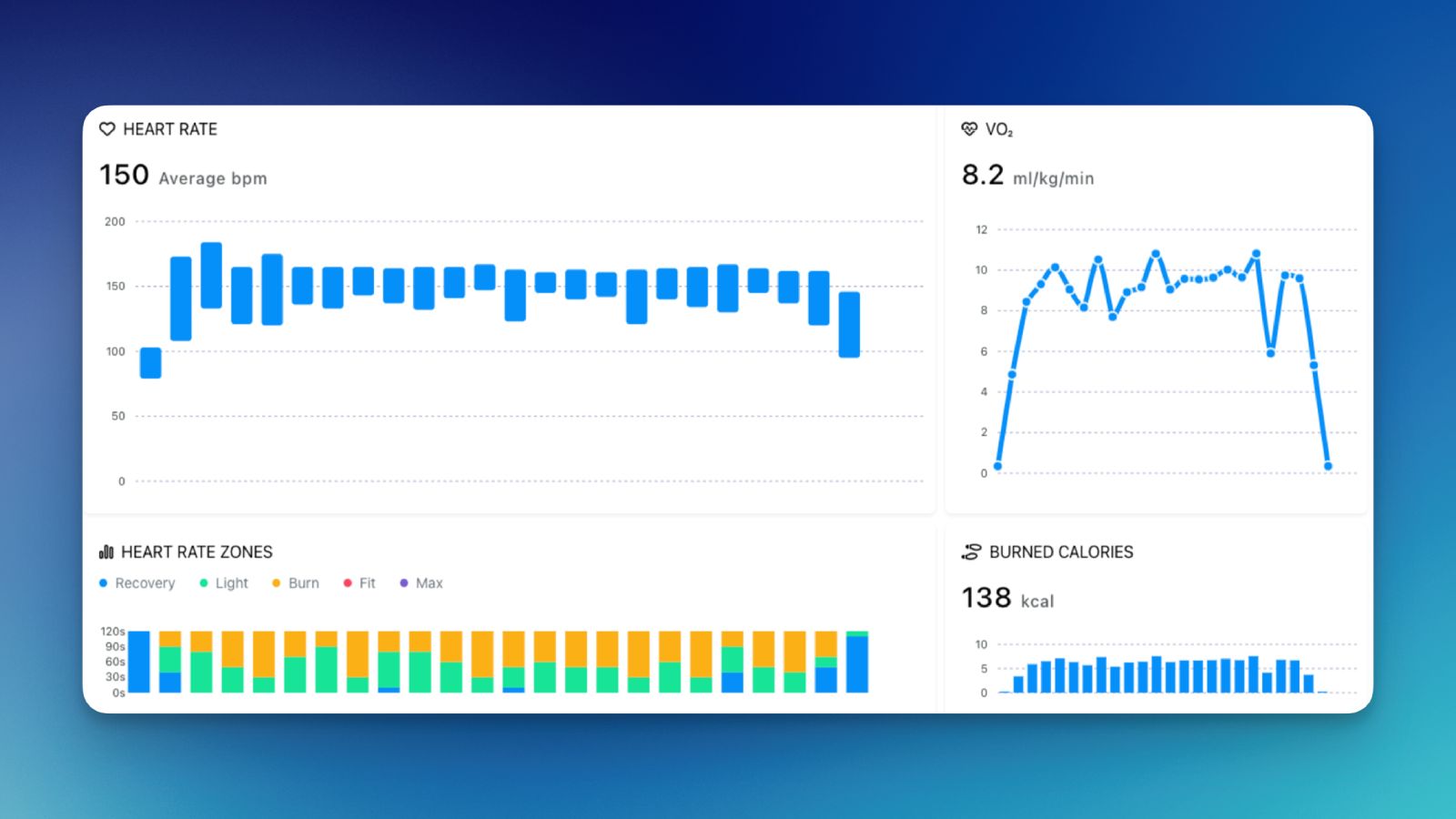
After completing sleep apnea monitoring at home, it becomes important to understand the scoring and interpretation of results. Home sleep studies usually check various parameters. These include breathing patterns, blood oxygen levels, heart rate, and total sleep quality. Each one assesses whether sleep apnea is present and how serious it is. For instance, the apnea-hypopnea index (AHI) is calculated, with specific values reflecting severity. An AHI of 5-15 shows mild sleep apnea, 15-30 indicates moderate, and over 30 points toward severe sleep apnea.
It is crucial to go over your findings with a healthcare provider. They can explain how the data fits into your health and symptoms. Professionals help to understand how results relate to your nightly experience or other health conditions. This conversation also brings to light any potential risks linked to sleep apnea, which helps in treating the condition holistically.
Your study results play a big role in treatment options. When the diagnosis of sleep apnea is established, providers may suggest adjustments like weight loss or change in sleep posture, or even suggest devices like CPAP machines. Sometimes, surgery options are available. Grasping the meaning behind your results aids in managing your health and improving sleep quality.
As you assess the findings, think about how they connect to treating sleep apnea. Gaining the right support and knowledge is vital for your sleep health. However, it's just as important to be aware of the limitations of home sleep studies, which we will cover next.
Advantages and Limitations of Home Sleep Apnea Tests
Home sleep apnea tests give major advantages. They help patients manage sleep health in a cheap and easy way. One main benefit is the cost savings. HSATs cost less than lab tests. They’re a good choice for people without full insurance coverage. Also, patients can take these tests at home. This helps reduce the stress that comes from sleeping in strange places.
Another big benefit is comfort. Many people feel relaxer and calm when they sleep in their own bed. This can help show true nightly sleep patterns. Studies show, many patients like home tests better than lab tests. This preference can lead to better results in sleep apnea monitoring.
But HSATs also have limits that need checking. A big limit is their accuracy. They might miss mild forms of sleep apnea. These tests focus on more serious cases. Thus, they may not catch subtle signs of sleep issues. This can lead to patients not getting the care they need.
Additionally, HSATs might not give complete information about other sleep issues. If problems continue, patients need to know when to get more tests. Meetings with health experts might be needed for thorough evaluations. This is especially true if test results show sleep apnea but daytime sleepiness still happens.
In summary, home sleep apnea tests have clear benefits. But they should be the first step in sleep apnea monitoring. They should not fully replace professional checks. For those with ongoing problems, more tests and expert help are needed for effective sleep health management.
Connecting with Health Professionals for Monitoring
The rise of telemedicine and wearable technology has made sleep apnea monitoring easier than before. Companies such as Aidlab are leading this change. They use advanced tools to help doctors engage with patients remotely. This method lets health professionals monitor sleep patterns and AHI values in real-time, promoting better management of sleep apnea.
It is important to engage with health professionals for ongoing care, especially in understanding the data from home sleep apnea monitoring devices. These experts provide important insights into the results, guiding patients to find effective treatment options for their conditions. Teaming with healthcare specialists helps patients grasp their sleep issues better, allowing informed health decisions.
Platforms like Aidlab Teams offer big advantages for ongoing patient engagement and data precision. Patients can send their monitoring results to healthcare providers easily. This way, any alerts in sleep patterns are dealt with swiftly, allowing treatment adjustments when needed. Continuous engagement not only boosts data accuracy but also supports a personalized method for managing sleep apnea.
In conclusion, using modern technology along with professional healthcare services is key for effective sleep apnea monitoring at home. By utilizing telemedicine and collaborating with health professionals, patients can ensure proper monitoring of their condition, ultimately leading to better health outcomes.
Conclusion
In summary, sleep apnea monitoring at home helps you better understand your sleep patterns. We covered the need for recognizing sleep apnea, types of monitoring devices, and how to conduct sleep tests correctly. We also talked about evaluating sleep study results, including the pros and cons of home tests. Connecting with healthcare experts is crucial for ongoing monitoring.
You have the information. Now, start researching suitable sleep monitoring devices. Consider scheduling your home sleep test. Use the knowledge for improving both your sleep quality and overall health. Remember, monitoring plays a key role in managing sleep apnea.
Prioritizing sleep apnea monitoring can promote healthier sleep habits. This leads to better quality of life. Stay proactive in seeking the right solutions that fit your individual needs.